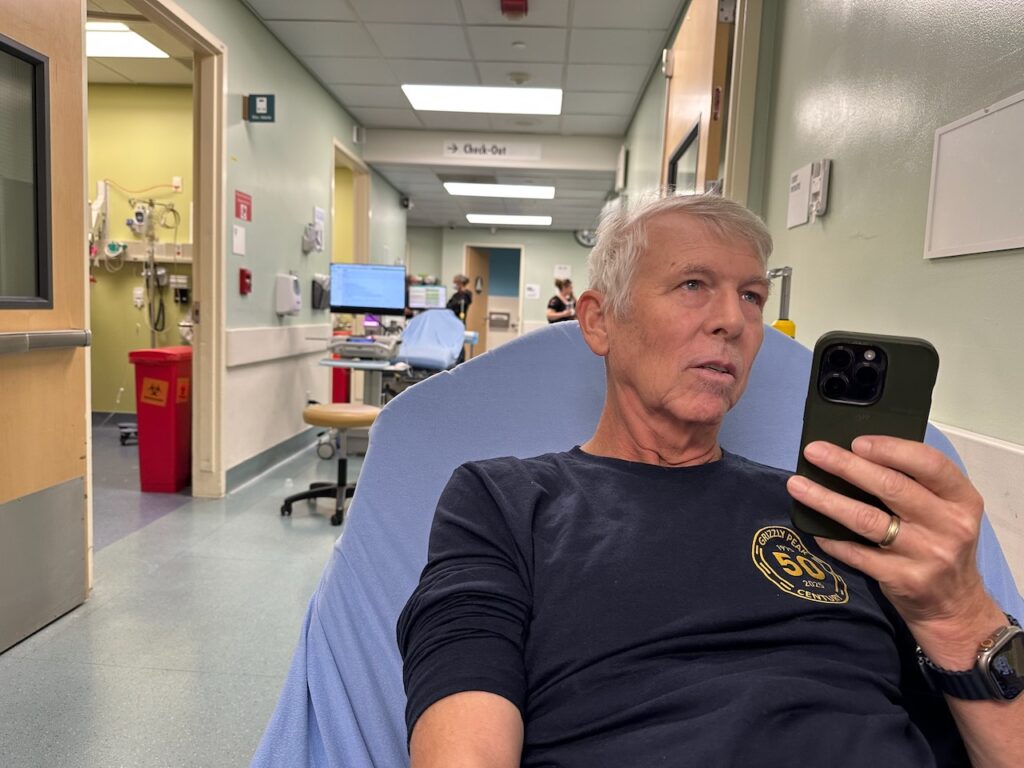
When my treatment ended in late May, the next question became “How can we be sure if we got it all?” The surprising answer was “There’s so much swelling during treatment, and it’s too easy to mistake swelling for tumors, so we have to wait three full months before doing another PET scan.”
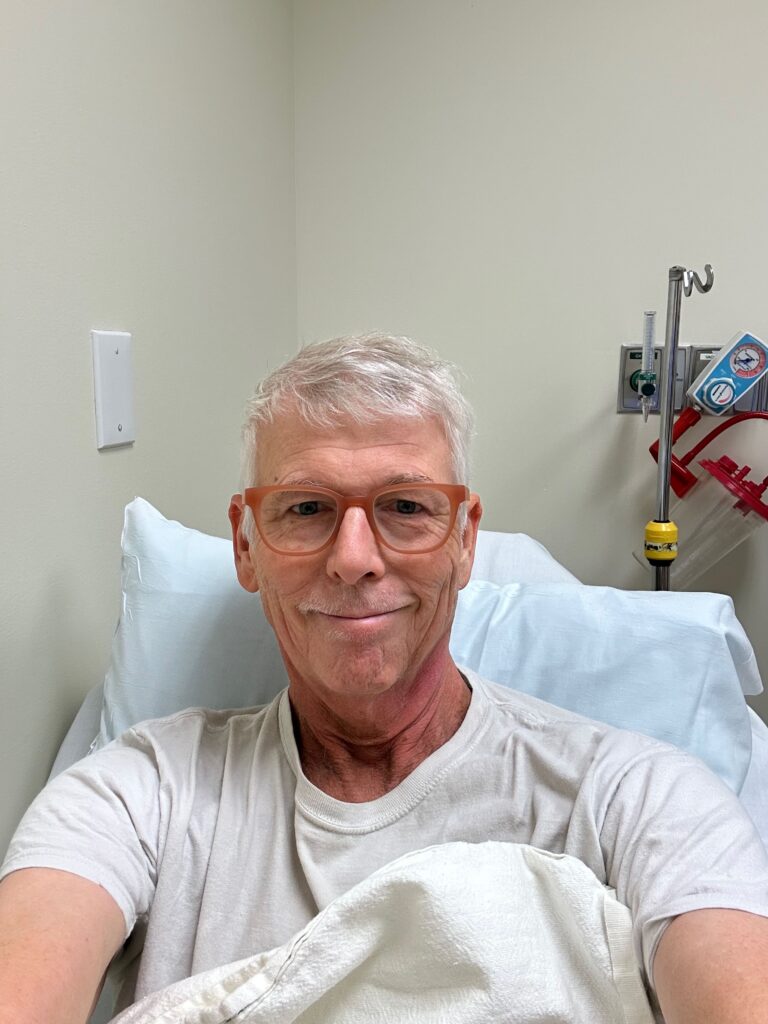
That day finally came yesterday. Half an hour on my back in the giant scanner (this one silent, unlike the crazy noisy MRI) and then a 24-hour wait for analysis. Today I met with the head of oncological surgery at Kaiser for the analysis. Short version: All clear! No sign of any tumor remains in my head, neck, or throat, and all former tumors are thoroughly dead and gone (or withered to nothing).

It’s hard to describe what it felt like to get this news, after everything we’ve been through since last March when I was first diagnosed. Saying “I’m cancer free” makes me start to tear up a bit now, just like saying “I’ve got cancer” did six months ago.
I knew in advance that my P-16+ variant responds very well to chemo-radiation, and that my chances were very good for full recovery, but that glimmer of doubt always remained in the back of my mind, making me nervous that I could have been in for a series of recurring cancers or something. I know that not all cancer patients are nearly this lucky, and I feel incredibly grateful to be at this point.
I’ll have to visit the doctor every three months for the next year, and then every six months for several years after to be sure, but for now, it appears we are out of the woods. Unfortunately that’s not quite the case with my remaining symptoms:
- Foggy headed / issues with word recall
- Low red & white blood cell count, plus platelets = low energy, dizzy spells, etc.
- Weight loss (I’m still down 30 lbs, and having trouble putting any back on!)
- Cotton mouth due to nuked saliva glands (this will get somewhat better over time, but is going to be more or less permanent)
- Sense of taste still only restored to around 50%
But the doctor was optimistic about every single one of those as well, and in fact thought I was doing incredibly well on each of those five counts for being only at the three-month mark.

So… huzzah! I didn’t quite jump and click my heels on the way out of there, but felt like it.
I just want to thank everyone from the bottom of my heart for all of the love and support you’ve shown over the past six months. It’s been an incredible ride that I never foresaw myself, but I’m pretty much out the other side now, and incredibly grateful – to my family, to my extended circle of friends, to medical science, and to at least one example of fantastic health care in the U.S.