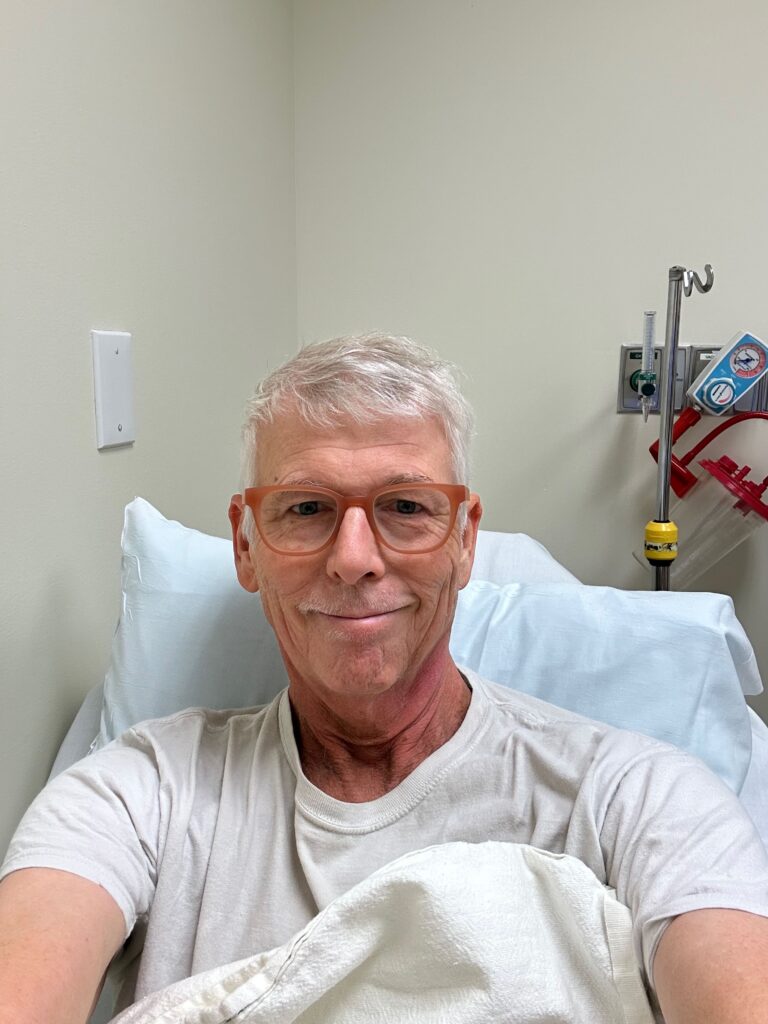
The feeding tube was essential for a period of about five weeks at the end of radiation, and for the few weeks after. But by July 3, I was once again able to get through a whole day on oral nutrition alone, without the need for tube feeding. The “deal” with my doctors was that if I could go for two whole weeks without using the feeding tube, I could lobby to have it removed.
My taste buds are still at around 50%, and eating food still takes a lot of work due to my reduced chewing surfaces and the lack of salivation, but I’ve been increasing the variety of inputs daily and am back to something resembling a “normal” diet (though I weirdly still don’t feel much attraction to meats and have been eating mostly vegetarian for months now). So I was super stoked to be able to return to the radiologist’s office today to have the feeding tube removed!

Good riddance. It feels like a fifth arm that’s been hanging out on my torso for the past month+ was just lifted away. It’s been a bit irritating the whole time, and I’m so looking forward to that healing up. Symbolically, it just feels like a big step on the journey.
The other development is around the mystery anemia I talked about in the last post. Technically, anemia is defined as a decrease in red blood cells, whereas what I’ve got is a decrease in red, white, and platelets, which is defined as cytopenia, not anemia. We’ve also been able to determine via more advanced blood tests that there is no shortage of iron or B12 in my system, which means there is no advantage to me taking any sort of supplements or vitamins.
If my blood counts get low enough, I could become a future candidate for a blood transfusion, but they currently are not, and are in fact moving in the right direction all on their own. The good news is that I am experiencing light-headedness less often and less intensely as days go by – I can feel myself getting better. Doctors now think that I am simply recovering from chemo more slowly than expected, but that there is nothing we need to do right now, except to do regular blood labs and to watch those counts creep up on their own. As long as they keep heading in the right direction, it’s all good.
So my remaining issues are:
- Cytopenia (getting better on its own)
- Diminished sense of taste (will probably mostly return within about a year)
- Dry mouth (salivary glands may never heal)